Those who understand the dynamics of psychological abuse know first-hand that the most effective abusers make you blind to the abuse. They teach you to reinterpret your surroundings, ignore your intuitions, and walk willingly, enthusiastically, into your own powerlessness.
If you truly understood how the field of psychiatry, as a whole, has held a chloroform-soaked rag over our humanity, you would be shaking with anger. Actually, utterly shaking.
In addition to gaslighting, clever abusers will offer something to create the illusion of power (which in the case of psychiatry is a little pill), so that as long as you hold it, you will think they’ve empowered you. In reality, they go on pillaging your world on a scale even they cannot fully grasp, creating a pervasive, lasting culture in which any signal that something is wrong becomes a knee-jerk trigger for you to dig down further into your own grave.
Consider this. Many drugs prescribed for depression increase the risk of suicide and work less effectively than placebos.1 This is evident in the data, but to fully grasp the significance, visualize the people in the numbers. There are people in our world who took pills from the industry of psychiatry, pills that pharmaceutical researchers knew worked no better than capsules of sugar, and instead of “getting better,” died by their own hand. If you are not horrified, you are misinformed.
At the root of this nightmare is a paradigm–a broad, unconscious worldview–that psychiatry has built and maintained so expertly that every new recruit embraces it as doctrine: the medical model.
The medical model is a set of assumptions about emotional suffering. About ordinary human suffering. When we look at the causes of suffering, the medical model provides a set of assumptions about what those causes are allowed to be. They form a starting point. The medical model says that emotional suffering is a medical problem. With medical solutions.
Speaking of assumptions and solutions, this past summer, I presented my oldest son with a toy, a cube composed of many smaller, wooden cubes all linked together by one long string (the “snake cube,” I think it’s called). Once the cube is unraveled, putting it back together is a challenge, because the string which connects them constrains the angles they may form when reassembled.

The puzzle looks like child’s play, and when I struggled to solve it, I was a little embarrassed. My oldest son, who just turned 20, is studying quantum physics at Caltech, one of the most competitive universities in the world. He once spent a week teaching himself C++ and then programming an interactive, three-dimensional world like Minecraft from scratch. That’s the sort of thing he does for fun. He spent hours fussing with the snake cube puzzle and could not reassemble it. I’ll admit, that made me feel better about my own defeat.
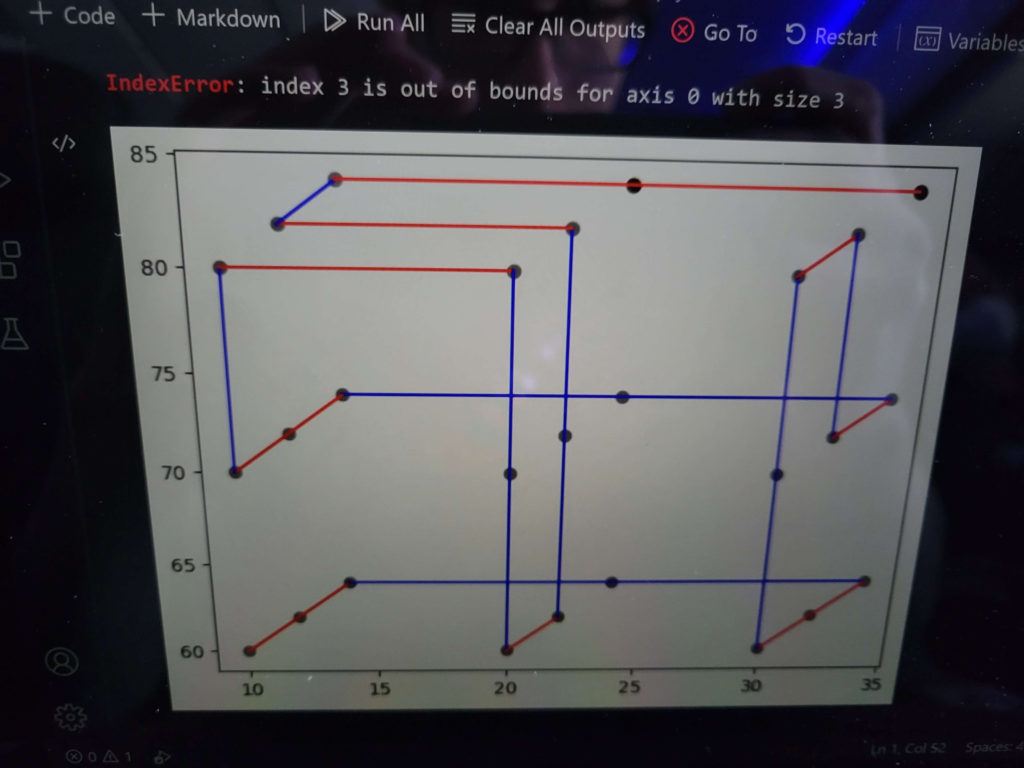
On a flight back to Caltech, my son wrote a program in Python to solve the puzzle. The program output a visual display of the solution on a 3 x 3 x 3 dot grid (representing the position of each block in the reassembled cube).
What I noticed, after having fussed with the puzzle myself for many hours, was that the solution had a feature which challenged my assumptions. One of the segments of smaller cubes had to be awkwardly folded inside another segment. Without being fully aware of making any assumptions at all, I had assumed that the solution would look elegant and feel intuitive, and I never even considered that I needed to jam a portion of the puzzle inside another portion. Actually doing so with the physical cube was not easy.
If you’ve ever tried to solve a riddle or a complex puzzle, you know that the solutions are often invisible until you question your deepest assumptions. The medical model is the set of assumptions no psychiatrist can question without being pushed out of the field. They have been trying for decades to solve the complex puzzle of human suffering, and they will continue to fail, because they are not allowed to question the medical model, and that model is the veil. Real solutions lie behind that veil in the awkward, inelegant, unintuitive messiness of human experience. When someone is suffering, it usually means we need to create a better world.
To frame this another way, imagine doing a criminal investigation after diamonds at a jewelry store go missing. Imagine a worldview that says that every time a jeweler is suddenly missing their gems, even if the windows are shattered and locks broken and footprints lead from the door to the vault, one must find just one primary cause, and that cause must be internal. We cannot even begin to entertain the possibility that a thief broke in and stole the gems. The fault must lie inside the store.
Even if we do admit that a thief may be involved, we can’t focus on that. The worldview says it’s irrelevant, a tangential matter outside the purview of the investigation. The solution will never be to apprehend the thief. The solution is constrained to be something internal with explanations and storylines that make the loss of the gem solely an internal event.
Imagine a detective who goes into every robbed jewelry store and tells them that their problem is this, and this alone: they just aren’t making enough diamonds. Then sells them a tool for making more and more diamonds!
What would you think? I can tell you what I would think. I would think they are working with the thief!
I’ve been reading some articles lately on the failures of the medical model, and I have to take such content in small doses. I read the book, Mad in America, by Robert Whitaker when it was first published, around 2002. I re-read it when I entered a graduate program in psychology at the University of Wisconsin, Madison. At that time, I still had the goal of finding ways to ease human suffering regardless of circumstances. That seemed like the holy grail—unconditional happiness.
When you endure trauma, major losses, and challenges building a life from the dirt up, you come into direct contact with social and political powerlessness. The most tantalizing solution is one you can control completely on your own, an internal one. I’d already rejected psychiatry as having any remotely appropriate solution, but I was still caught up in a version of the medical model, one in which the body, mind, and heart are like machines, and when the gears are signaling trouble, one just needs the right wrench to throw into them and stop their painful turning. It’s taken a very long time for me to completely let go of the idea that I can somehow gain full control over the causes of emotional suffering and never hurt again.
What’s especially challenging is that the suffering evoked by trauma, loss, and hardship makes life even harder by compelling changes in behavior that are out of alignment with the system you must continue to live and work in. I would say the suffering is crippling, but I’ve changed my mind on that. I don’t think it’s crippling at all. Emotional suffering motivates behaviors designed to transform the situations that evoked it, but we are embedded in systems that make those same behaviors personally detrimental. The prolonged rest compelled by depression, for example, would seem far less crippling if we weren’t required to work long hours every day in an office that discards us the moment we become useless to the bottom line.
It has taken me decades to fully appreciate just how messed up the medical model truly is. But I’m glad. Every waning of the medical model in my personal worldview has been accompanied by a waxing of compassion.
The hardest part about acknowledging that you’ve been disempowered is letting go of the illusion of empowerment (in this case, hope delivered in the form of pills). Until you have some alternative, acknowledging the abuse feels worse than continuing with the illusion. I would offer, however, that becoming angry at abuse, either personal or systemic, is the first step toward real power.
Recommended Reading
If “abuse” seems like too harsh a word for the marketing of psychiatric drugs, there are decades of articles, books, research, and activism that may change your mind. Something to start:
Once Radical Critiques of Psychiatry are Now Mainstream, So What Remains Taboo?
By Bruce E. Levine
From the article:
It remains taboo to challenge whether or not medicalizing our emotional suffering and behavioral disturbances is the best model of care. Such a challenge, as noted, is not only an existential threat to establishment psychiatry but a financial threat to Big Pharma and a mainstream media dependent on Big Pharma advertising dollars. Even more significantly, such a challenge is a political threat to the ruling class which prefers “individual defect” explanations for emotional suffering and behavioral disturbances—rather than explanations that take seriously the direct and indirect effect of an alienating and dehumanizing society.
Eighty Percent of the Population Will Get Treated for Mental Illness in their Lifetime—and They’re Worse Off Afterward
By Peter Simons
Mad in America: Bad Science, Bad Medicine, And The Enduring Mistreatment Of The Mentally Ill
By Robert Whitaker
The Emperor’s New Drugs: Exploding The Antidepressant Myth
By Irving Kirsch, Ph.D.
Footnotes
- Why antidepressants are simply a confidence trick: A leading psychologist claims taking sugar pills would work just as well ↩︎
Image credit: Image by wirestock on Freepik

